In an earlier post, I asked whether stay-at-home orders were successful in reducing Covid-19 mortality and preventing the collapse of hospitals. To be able to compare costs and benefits of policy interventions, we need to understand both. This post shall shed light on the costs of lockdown measures, especially those health-related costs. As before, I will put the focus on stay-at-home restrictions, but I will touch on the effects of other Covid policies that are closely related. Please note that I first published most of this text on 29 July 2021 and I only did some minor revisions before publishing it in this blog format. Some numbers might therefore not be the latest and most relevant studies that were published recently are missing.
It is important to keep in mind that the evidence I refer to in the following is necessarily incomplete as lockdowns have affected every aspect of our lives. “The costs include not only measurable outcomes such as job loss or drug overdoses, but intangibles such as shattered dreams, social starvation, and existential despair. These costs are no less real for being difficult to quantify.” (reddit user freelancemomma) The variables that lockdowns are intended to affect are not too hard to measure: Infections, free hospital beds, deaths. The costs are manifold and hard to quantify. It is equally difficult to establish causation, i.e. attribute them to lockdowns, specifically because the pandemic itself has side effects that go beyond the direct costs of infections, like the widespread fear of the virus.
Economic costs of lockdowns: Saving lives by saving the economy
There are several serious undesired side effects of Covid-19 containment policies that I would like to address here shortly even though they are not directly related to stay-at-home orders: The economic costs of stay-at-home orders are probably small compared to the costs of business closures and restrictions and border closure. But as these measures were often applied together with stay-at-home orders and were jointly branded as “lockdown” policies, they are closely related. For an overall assessment of the effect of non-pharmaceutical interventions as a response to the Covid-19 pandemic, it is of utter importance to take the economic effects and economics-related health effects into account. Economically illiterate social media warriors have not ceased to exclaim that the priority should be to “save lives, not the economy” without taking into consideration that people live off the economy. Even in rich countries such as the UK, Denmark, and Germany, evidence shows that poor people die several years earlier on average as compared to rich people. A policy that makes people poorer might thus not be very suitable to save lives in the long run.
Economic stress and unemployment are risk factors for many severe illnesses. Researchers from the University of Oxford have calculated that the financial crisis has caused more than 10,000 additional suicides between 2008 and 2010 across the US, Canada and Europe. And suicides are just the tip of the iceberg. Unemployment is strongly associated with worse physical and mental health (see e.g. here and here).
In rich countries, the costs of business closures can be made up for by government transfers, but not the psychological effects of unemployment, and in this case, of the message that they are officially branded as “inessential” for the society. Complete compensation of lost income is not feasible in poorer countries and even in richer countries the precariously or unofficially employed do not benefit from compensation schemes. A brothel owner in Germany might be financially recompensated by the government, but the unregistered prostitute in the street cannot claim any financial benefits. Farmers were allowed to continue working and Germany was quick in creating a website where German students could register as farm workers. At the same time, foreign seasonal labourers lost their planned income of an entire season. Just like there are clearly defined risk groups for a serious Covid-19 infection (the elderly and those with certain medical conditions), there are economic risk groups for serious lockdown harms.
The connection between wealth and health is much more extreme in poorer countries. Lockdowns have destroyed the livelihoods of millions in developing countries where little social safety nets exist. It should be taken into account that even “our” containment measures in the richer countries have detrimental effects on the world’s poor. Business closures in Europe disrupt global supply chains, at the expense of workers in Asia who are laid off. Also think of countries like Thailand that depend heavily on tourism, a sector that was crushed by travel restrictions. Dr. David Nabarro, WHO’s Special Envoy on Covid-19 made clear in October 2020 that the WHO does not advocate lockdowns as the primary means of control of this virus due to the effects on poverty and child malnutrition. Oxfam warned that lockdown-related hunger could claim more lives than the virus itself. Hunger and malnutrition have been widespread in 2020 among children who would, under normal circumstances, receive food at school. On the peak of school closures, the World Food Programme counted 369 million children missing out on school meals globally. In 2021, the FAO reports that after five years of virtually no change, the global prevalence of undernourishment has increased 1.5 percentage points in one year. Note that we are touching very sensitive ethical questions here: How many starving children are okay to save how many 80-year-olds from dying? My personal answer would be zero.
It will probably never be possible to make an exact calculation of how many people died earlier as an effect of Covid-19 containment policies and how many they saved from dying earlier because we have no counterfactual. Had the world not locked down, people would have changed their behaviour nonetheless. An economic crisis could have emerged only from the pandemic itself and individual, voluntary reactions to this threat. For instance, people would likely travel less even if there were no travel restrictions. Nonetheless, the economic turmoil would have certainly been much less severe without drastic authoritarian containment measures.
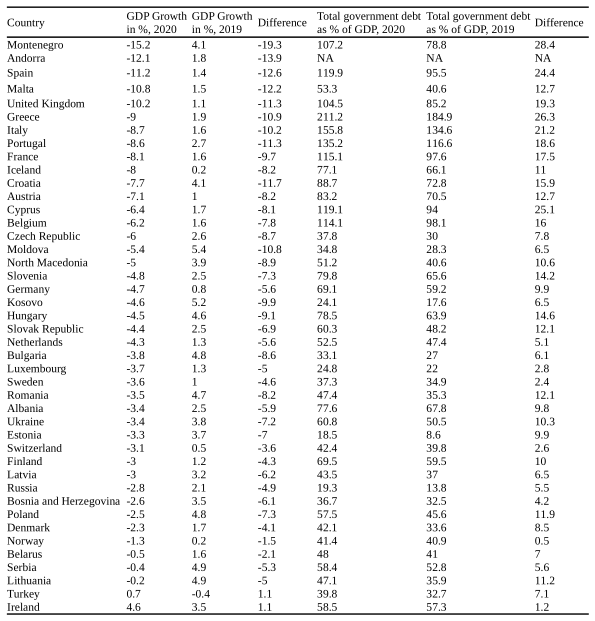
Turkey and Ireland prove that it is not impossible to grow economically despite tough restrictions, yet it is striking that all countries on the ranks 3 to 8 had comparably softer restrictions, namely, no stay-at-home orders. The correlation between less restrictions and better economic isn’t perfect, but it seems much clearer than any correlation between restrictions and less mortality.
Governments prevented economies with the largest borrowing since World War 2. According to IMF data, global debt (public and private) rose from 227 to 256 percent of GDP in 2020. The table shows the increase in total government debt as percentage of GDP differences for European countries. Again, we see countries with fewer restrictions, like Norway, Sweden or Switzerland performing better, while countries with tough restrictions like Spain and Italy can be found among the countries where public debt increased most. Of course, restrictions clearly aren’t the only factor of importance here. It is mostly the countries where public debt was already high before the crisis that showed the largest increase. We might also want to interpret this in a way that countries that traditionally had been less prone to take up debt decided against tougher restrictions on this ground whereas political leaders in economies that were used to high debt were more willing to impose costly restrictions. In any case, this large increase in public debt puts an additional burden on younger generations.
Health beyond Covid-19
Non-pharmaceutical interventions to curb the spread of coronavirus have had tremendous implications for physical and mental health. An important health-related side-effect of lockdown measures has been an increased reluctance of people to seek medical care. This could have been caused by the fear of getting infected at the doctor’s practice or by a wish not to contribute to an expected overwhelming of the health system. But given that primary care contacts dropped at a time when health systems were clearly not overloaded (though expected to) it is likely that some people decided not to see a doctor due to the social pressure of the virtual #stayhome mob. It was after their furore turned into policy that primary care contacts in the UK for nearly all analysed conditions dropped significantly (Mansfied et al. 2020). By July 2020, contacts for nearly all analysed health conditions had not recovered to pre-lockdown levels. The conditions included in the study covered several mental conditions (e.g. depression, self harm, eating disorders) but physical conditions, too, such as heart failure and myocardial infarction. It is unlikely that the lockdown caused the number of heart attacks to fall from one day to the other. In the words of Mansfield et al. “it is more likely the reduced primary care contacts we saw represent a substantial burden of unmet need (particularly for mental health conditions) that could be reflected in subsequent increased mortality and morbidity.” As I will address further below, mental health problems were seriously exacerbated by the lockdown thus the number of people seeking care should have risen rather than fallen.
The same pattern was observed in other countries, e.g. in Germany where stationary cases in hospitals went down by 30% between March and May 2020 as compared to the normal level. Between mid-March and early April of 2020, hospital admissions for heart attacks fell by 28% in Germany and for strokes by 15%. This development is more likely to reflect social trends rather than rational thinking given that less than two percent of all beds were occupied by Covid-19 patients in the respective time period thus there has been no reason not to go to the hospital with a heart attack out of fear the hospital might be at full capacity. A comprehensive summary of the evidence of first-wave restrictions on cancer care is provided by Heneghan et al. (2021). Revising this text in February of 2022, I should add that health care providers have still not cleared the backlog. In the United Kingdom, the number of people waiting a year or longer for NHS treatment has increased 200-fold as compared to pre-pandemic levels and is at a record high.
Many of the most striking public health problems of this age are related to an unhealthy lifestyle. As ever more people spend most of their day sitting, obesity has become a pandemic over the last decades. According to WHO estimates, more than half of Europeans were overweight in 2008 and more than a fifth was obese. As the WHO Regional Office for Europe writes on their website: ”Participation in 150 minutes of moderate-intensive aerobic physical activity each week (or equivalent) is estimated to reduce the risk of ischaemic heart disease by approximately 30%, the risk of diabetes by 27%, and the risk of breast and colon cancer by 21–25%. In addition, it has positive effects on mental health by reducing stress reactions, anxiety and depression and by possibly delaying the effects of Alzheimer’s disease and other forms of dementia. In Europe, estimates indicate that over one third of adults are insufficiently active.”
As we see, physical activity is beneficial for preventing some of the most prevalent physical and mental health issues. This is not limited to ambitious exercise. A simple walk in the park already brings about similar benefits. See for example this article for an incomprehensive list of health benefits that come with spending time outside). But without citing any more articles, I would assume that it has long been common sense that regular physical activity or exercise, fresh air and the right amount of sunlight exposure are beneficial to health.
It is hardly needed to cite any scientific studies to know that physical activity declines when people are recommended to, pressured to, or, as in most countries, forced to stay home. For numbers, you can see, for instance, Wilke et al. (2021) who performed a multinational study in 14 countries. Moderate-to vigorous physical activity declined by 41% and vigorous physical activity declined by 42.2% in April and early May of 2020 as compared with pre-lockdown levels. Wilke et al. find a correlation between the Containment and Health Index (CHI, the stringency index mentioned in the last post calculated with the OxCGRT data) and reductions in physical activity. They note Spain among the outliers due to its low CHI index and high reduction in physical activity which, in my eyes, shows the inappropriateness of the CHI as a measurement for the severity of lockdown as Spain imposed some of the strictest restrictions on movement of all European countries.
Largely neglected in general debate, the world is facing a second pandemic of mental nature. It is unclear to what extent the mental pandemic is caused by fear of the virus itself and to what extent it is caused by political and social changes as a reaction to the pandemic. Looking at statistics on psychopharmaceutical prescriptions, it comes clear that the mental health pandemic was ongoing for years when the pandemic started, but it worsened a lot over the course of 2020: Covid-19 Mental Disorder Collaborators (2021) (https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02143-7/fulltext) conducted a systematic review of data reporting the prevalence of major depressive disorder and anxiety disorders during the Covid-19 pandemic published between January 2020 and January 2021. They found that both the reduction in mobility and daily SARS CoV-2 infections in a country were associated with a higher prevalence of anxiety and major depression. Females and younger age groups were affected disproportionally. Overall, the authors estimate that the global prevalence of major depressive disorder increased by 27.6% over the studied time and the prevalence of anxiety disorder by 25.6%.
In a representative YouGov survey conducted in November 2020 in 16 countries and territories, between 44% (Germany) and 65% (United Kingdom) of respondents reported that the pandemic had detrimental effects on their mental health. More than 42% of people surveyed by the US Census Bureau in December reported symptoms of anxiety or depression in December, an increase from (not of!) 11% the previous year. UK adults reporting symptoms of depression almost doubled from 10% before March 2020 to 19% in June 2020.
The NGO Deutsche Depressionshilfe (German Depression Aid) conducted a representative survey in June and July of 2020 among 5,178 people between 18 and 69 years old and living in Germany. 1,094 participants have been diagnosed with depression at least once in their life and 197 suffered from acute depression. The fear of infection with SARS-CoV-2 was equal among the subsamples of depressed and the entire sample (43% vs. 42%), but in the sample of acutely depressed, a higher percentage (retrospectively) reported negative feelings about the first four weeks of lockdown (74% vs. 59%). Also, while the majority thought that social cohesion increased during the first four weeks of lockdown (54% agreement), the majority of depressed did not agree to that statement (44% agreement). In June and July, 68% of acutely depressed felt negative about the current situation as compared to 36% in the entire sample. In a second survey conducted in February 2021, equally representative for 18- to 69 years olds in Germany, 89% of acutely depressed reported that they are missing contacts to others and 87% reported not having sufficient exercise.
With the worsening of public mental health, treatment worsened too. In Germany, it was already difficult to find a therapist before the pandemic and waiting lists were long. The pandemic further exacerbated this problem. In both surveys of Deutsche Depressionshilfe, more than every second patient suffering from acute depression reported cancelled therapy sessions or other constraints to therapy (Reich et al. 2021). In Wales, people referred to talking therapies fell by a third compared to pre-lockdown times while the prescription of antidepressants increased.
It is incredibly hard to properly estimate the mental health implications of lockdown measures. Most studies on mental health rely on typically rather small samples of volunteers. Everywhere, different non-pharmaceutical interventions were applied at the same time or in quick succession thus making it difficult to isolate the effect of stay-at-home orders. Additionally, huge mental stress cannot only arise from the fear of the virus or from lockdown measures, but from the fear of anticipated lockdown measures too. Personally, I can report that I spent many weeks in distress caused by the fear of being confined and the fear of people around me pushing for confinement.
To be fair, we have to acknowledge that some measures that came with the “lockdown” label had a positive effect on some people’s mental health. Many studies on the subject (e.g. Pieh et al. 2021, Ahrens et al. 2021) have found very heterogeneous mental health effects of non-pharmaceutical interventions: While some were affected negatively, others benefitted from reduced levels of stress due to working from home or not working at all.
Evidence from Germany suggests that (self-reported) stay-at-home orders are associated with higher levels of depression and anxiety among younger adults in particular (Benke et al. 2020). The German situation was particularly useful for such an analysis as some states issued a stay-at-home order and others did not. As stay-at-home orders in Germany during the first wave allowed outdoor walking at all times (except in a few villages), the effects are likely to be smaller than in countries that did not allow these exceptions. Reich and Klotzbücher (2020) make use of data from Germany’s largest telephone and online crisis helpline service Telefonseelsorge. Reich and Klotzbücher had access to anonymised data on all recorded contacts from 1 January 2019 to 10 May 2020. They find a significant increase of calls of about 20% following the national “lockdown” in Germany. They control for Covid cases on a state level in order to separate the effect of the lockdown itself from the effect of the spread of the virus. Reich and Klotzbücher considered regional differences in what “lockdown” meant, i.e. whether there was a stay-at-home order in place, whether it was allowed to have a picnic in public or whether it was allowed to visit acquaintances at home. Only for four states, they could assure that helpline calls were not redirected across state borders so that it was possible to definitely say where the calls were from. These were four of the five most populous states: Northrhine-Westfalia, Bavaria, Baden-Württemberg and Hesse. Among these states, they found that the most substantial increase in helpline calls was observed in Bavaria, the state with the strictest lockdown rules followed by Hesse, Northrhine-Westfalia and Baden-Württemberg – in the exact order of strictness of lockdown measures. After the fourth week of lockdown, helpline calls slowly started to decrease again and at the end of April, Reich and Klotzbücher found no statistically significant difference anymore. Not only the timing of the spike in helpline calls suggests that the cause are social distancing policies rather than fear of the virus or the economic crisis: There was no increase in talks about physical health or financial problems, but a significant increase in topics such as loneliness, depression, and anxiety. They also point to the fact that in the German-speaking regions of Switzerland, where social distancing measures were less strict, there was no significant increase in helpline calls (Brülhart and Lalive 2020)
Further evidence for adverse effects of lockdowns on mental health is provided by Pieh et al. (2021) who found the prevalence of depressive, anxiety, and insomnia symptoms to be significantly higher in the UK four weeks into the first lockdown relative to pre-pandemic epidemiological data. In Austria, Pieh et al. (2020) found the prevalence of depression and anxiety to be higher four weeks into the lockdown than in pre-pandemic times and found the lockdown to be especially stressful for younger adults. In the UK, the factor most highly associated with high anxiety during lockdown was loneliness. People who “often or always” felt lonely were almost five times more likely to report high anxiety than those who “never” feel lonely. Of course, stay-at-home orders and contact bans directly cause loneliness. Rossi et al. (2020) found high levels of post-traumatic stress symptoms, adjustment disorder, high perceived stress, anxiety, depression and insomnia associated with the first lockdown in Italy in a non-representative sample. In the United States, lockdowns were associated with a stark increase in drug overdoses. They jumped 18% in March of 2020, 29% in April and 42% in May (all compared with 2019) according to this Washington Post report. In Europe, drug overdoses are far less common. Drug use changed during the lockdowns, but it is not clear whether there is any causal relationship. According to Manthey et al. (2021), alcohol use has decreased in Europe while tobacco and cannabis consumption increased. There is a lot of heterogeneity though as some users reported drinking much more while others reported drinking much less. That there are no huge changes on average does not neglect the possibility of an increase in problematic consumption patterns among some groups. The OECD notes that 43% of surveyed persons in 11 OECD countries reported drinking more frequently during “lockdown” while 26% report drinking less. Drinking more was specifically common among women, parents of small children, people with a higher income, and people with symptoms of anxiety and depression.
Few studies have made cross-country comparisons of the effects of lockdowns on mental health. Brodeur et al. (2020) used Google Trends to check if people searched for mental health-related expressions more or less often after a lockdown was announced in a country or territory covering the United States and nine Western European countries. They found that around the announcement of lockdowns, searches for boredom and loneliness spiked. Searches for loneliness decrease throughout lockdown in Europe but not in the US. Searches for sadness did not increase immediately after the announcement of a lockdown but were on the rise until three weeks after a lockdown was announced. Surprisingly, searches for suicide fell in both regions. This is in line with Pirkis et al. (2021) who found that in 21 analysed countries, suicides either decreased or stayed constant between April and July 2020 as compared to pre-lockdown levels. It is important to keep in mind that suicides are seldom a spontaneous reaction to external conditions, but often the result of years of suffering, most commonly from depression. Even if lockdown measures have not caused an immediate spike in suicides, their effect on the prevalence of depression risks causing more suicides in the future.
Aside from the immediate physical and mental health deteriorations associated with lockdowns, the stress caused by fear-mongering public communication and extreme policy measures is likely to have devastating long-term effects. Of course, most people believe lockdowns were an effective means to control the pandemic. Many of these people may have experienced lowered stress levels during lockdown as they felt safer. But as I will highlight in one of the next posts, the public communication and policy that has been prevalent since March 2020 in most countries has lead many people to grossly overestimate both the social risk and their personal risk to fall seriously ill from Covid-19. Mislead policy increased stress levels in the first place which have then been reduced for some by lockdown measures. It shall not be underestimated how lockdowns can increase fear as people think the danger has to be extraordinary if such extraordinary measures are taken. So for those who believe in lockdowns, their effect on stress can go in both directions. It is likewise worth noting that for proponents of lockdowns, it can be encouraging to know that their sacrifices has a positive impact on the state of the world. For the (not so small) minority that is forced into lockdown against their will, it is straightforward that the measures mean extreme stress. Personally, I have been feeling constantly stressed since March 2020. As Schippers (2020) writes “acute stress in a healthy human is quite harmless, but stress that last for days, weeks, months or years can be harmful. It can result in a state of chronic systemic inflammation which in turn results in the development of chronic diseases.” and “chronic stress in advanced age will accelerate aging and dysfunction of the immune system.”.
Patients of care facilities were affected by lockdown measures well beyond the average. In my database of stay-at-home orders, I excluded regulations on quarantines of care facilities to be able to make comparisons for the general population. Elderly and handicapped people living in care facilities have been subject to quarantine even in countries where no population-wide lockdown measures were imposed. Conditions in care facilities have left room for improvement before the age of lockdown, but with Covid-19 restrictions, many care facilities have effectively turned into prisons. The enforced isolation is especially difficult to process for patients with dementia. Research from Italy and the UK, point at a serious worsening of symptoms among dementia patients. A survey among 950 experts in care homes and 1000 experts in ambulant care services in Germany found that the mood and life satisfaction of 74% of all care home residents has worsened during the pandemic. 82% of surveyed care home workers reported that a general ban on visits was imposed in their facility. Note that a big share of those who have died with Covid-19 were residents of care homes thus the lowered mood of surviving residents may be explained by these deaths to a certain extent. Yet, it is beyond doubt that the isolation that was enforced on care home residents had its toll on their wellbeing.
Pouso et al. (2021) is the only study I came across that explicitly acknowledges differences in lockdown stringency regarding individual outdoor movement. As they summarise: “Importantly for the COVID-19 crisis, research suggests that maintaining contact with nature during stressful life events, such as relationship breakdown or job loss, can “buffer” individuals against stress; with those living in greener areas reporting fewer mental and physical symptoms of poor-health during, and shortly after, the stressful event. It is also important that while ‘home’ is generally considered a restorative environment in psychological literature, during the COVID-19 crisis, school’ closures and the increase of telework might have compromised its restorative potential. Under these special circumstances, being able to maintain contact with nature from home might have had a relevant positive effect in mental health, compensating the loss of the restorative effect of the home, to some extent.” Pouso et al. distributed an online survey internationally and got 6,080 valid responses. Only including countries with at least 100 responses, they obtained a non-representative sample of 5,218 people from nine countries: Spain, United Kingdom, Germany, France, United States, Portugal, Italy, New Zealand and Mexico. They grouped countries into three levels with level 1 countries restricting access to outdoor public spaces (e.g. Spain), level 2 countries allowing for some outdoor activity (e.g. UK) and level 3 countries not restricting access to outdoor space. Which level a respondent’s region was in was self-reported by the respondent. They “found a clear negative effect of severe confinement on mental health, with people who had restricted access to outdoor public spaces (Level 1) more likely to show symptoms of mental health disorders than people who had partial (Level 2) or no restriction (Level 3) to access to outdoor spaces.” In countries with a strict lockdown, natural views as well as access to nature, e.g. in the form of a private garden, were associated with a lower risk of anxiety and depression. The Spanish subsample was analysed further and Pouso et al. found that a private garden or patio contributed more to mental health than a balcony. As with the economic effects of containment measures, we find a similar pattern of inequality here: People in urban environments without natural views and without a balcony are more likely to suffer mentally from being locked down than those who have access to land. A limitation of Pouso et al.’s study is that the sample is not random and highly educated people are particularly overrepresented as the sample was drawn using a “snowball” technique where the researchers sent the survey to their acquaintances with the demand to forward it. This is not uncommon of course, and you should generally be aware that much research, e.g. in the field of psychology, is carried out using samples of university students leaving people with lower formal education severely underrepresented.
Given the tremendous health benefits from physical activity and from experiencing nature, preventing people from going out is likely to have a devastating effect on public health. You should assume that policy makers worldwide would only take such a measure if its immediate benefits unambiguously exceed its risks. However, there has never been a plausible causal explanation or evidence for a significant infection risk when being outside keeping a distance towards others. Stay-at-home orders have been justified with their indirect effects: When you are not able to go out, you are also not allowed to meet anyone. On the other hand, most countries that did not implement stay-at-home orders have introduced strong rules on gatherings thus reaping the potential rewards of social distancing without the costs of disallowing individual exercise. Even when assuming that (private) social interactions do not reach the absolute minimum when only gatherings are banned and individuals can freely circulate, I doubt that the net effect on health of this extra reduction of social interactions would be positive. I think everyone knows moments in which meeting a friend is priceless. Especially in times of crisis, people may need a hug, a shoulder to lean on, or just someone to talk and cry. When the government regulates the maximum number of people who are allowed to meet, there are two breaking points: The first is when any restriction is set in place as it means that the government suspends the right of assembly. If a democratic government starts to suspend such a fundamental right, this has strong implications on the self-conception of the society and the relationship between the governors and the governed. But aside from political and philosophical questions, the immediate effects on the lives of most people are arguably negligible (except for some, e.g. event managers). The marginal costs of a reduction from 100 to 50, to 10, or maybe even to 5 people are fairly small, but the costs rise when numbers are becoming very low. When no more than 3 people are allowed to meet, two befriended couples could not meet anymore, for instance. I hypothesise that the marginal costs of reducing the number of people someone is allowed to meet from 1 to 0 has the highest marginal costs. Loneliness is not an enjoyable state for most people. And for suicidally depressed or for people with an addiction this one other person could save their life. Free individual movement probably ensures that those who do emergently need to see a friend (but do not want to bother to explain themselves to the police) will just do so despite it being prohibited. A stay-at-home order with a complete ban on meeting people outside the own household is certainly very harmful and almost certainly lethal for some people.
On top of the huge toll lockdowns take on people’s mental health with increased prevalence of anxiety, depression and substance abuse, interpersonal problems might be exacerbated by lockdowns: The combination of economic and social stress factors with lockdown policies have dramatically increased cases of domestic violence in almost all countries. For many, home is not a safe place and the freedom of movement to leave home at all times has been taken for granted by almost everyone until March 2020. For some, the loss of this freedom might only mean a minor annoyance, but for others, It puts them at serious risks. Being able to see a friend or even sleep at a friend’s place cannot only save the lives of some suicidally depressed but it can be the only rescue for people facing intimate partner violence.
While their freedom of movement has always been more restricted, children might suffer most from enforced isolation. While the overwhelming of hospitals never became a reality in Germany, the social response to Covid-19 has caused an overwhelming of the psychiatric system. The spokesperson of the German Professional Association of Pediatrics in May 2021 spoke of triage in psychiatric wards for children and adolescents: “There are psychiatric illnesses on a scale we have never experienced before. The child and youth psychiatries are full, there is a triage there. Those who are not suicidal and “only” have depression are no longer admitted at all.” It would be unfair to blame children’s poor mental health on stay-at-home orders, however, as most of Germany only experienced strict night curfews which do not affect children who are usually not outside after 9 PM anyway. Instead, we are probably seeing the side effects of school closures, mask mandates and an unprecedented campaign of fear. It is often stated that children are adaptive and therefore the closure of playgrounds and kindergartens would not cause excessive suffering. But clearly, there are boundaries to children’s adaptiveness. Complete isolation from other children for a longer period is unnatural and may seriously inhibit children’s development. For small children, there are developmental “windows of opportunity” in which they typically learn certain behaviours (similar windows exist for children’s immune system). Making up for the lost opportunities to learn and develop can be hard or even impossible. And we cannot know what it does to children to grow up in an environment of fear where the message they learn every day is that they are dangerous and every human contact is potentially dangerous. Joffe (2021) summarises:
“Especially concerning are the effects on children during “the early years” of life, increasingly recognized as the period of greatest vulnerability to, and greatest return on investment from, preventing adverse long-term outcomes that can have lasting and profound impacts on future quality of life, education, earning potential, lifespan, and healthcare utilization. The early years of life are a critical period when a child’s brain develops from social interaction and experiences, thus providing the foundation for their entire future life potential. During the pandemic children are being exposed to increased intimate partner violence, family financial crises, disrupted education, an increasing achievement gap (i.e., low-income families who do not have access to a computer, internet, space, food, and parental support cannot participate in online learning), loneliness, physical inactivity, and lack of support services (e.g., school lunches, access to early childhood services and aids for those with disability). These adverse childhood experiences have permanent impacts that cannot be compensated for by later improvements in social situations.”
Speaking of children, another cost of lockdowns that cannot be compensated for some is the missed opportunity to conceive children. Women have only a limited time to conceive children and their fertility declines significantly in their 30s and 40s. If a woman was kept from finding a partner due to social distancing policies or from seeing her partner due to travel restrictions, it could be too late to have children after lockdowns are lifted. This is another example of costs of social distancing policies that are impossible to capture in a statistic but are nevertheless real.
In summary, costs of stay-at-home orders are difficult to quantify as they coincide with costs resulting from the pandemic itself as well as costs of other policy interventions. There is clear evidence of stay-at-home orders and other interventions labelled as “lockdown” to have devastating effects on many people’s mental health with increasing rates of anxiety and depression. Furthermore, there is some evidence that substance abuse has risen among parts of society. The mental health effects of lockdown measures are not distributed equally. Several studies found younger people, including children, to be particularly vulnerable to suffer from mental health issues following lockdown policies. For strict stay-at-home orders, those without private outdoor access suffer significantly more than those with access to a garden. Another subgroup that suffered tremendously have been elderly people in care facilities and dementia patients whose symptoms worsened. Cases of domestic violence have spiked during lockdowns with reported cases probably only being the tip of the iceberg of aggravated within-household violence. Strict stay-at-home orders caused people to be less active which has potentially huge adverse effects on physical and mental health if lasting for a longer time. Another lockdown-related cost to physical health comes from skipped health check-ups and delays in treatment e.g. of cancer patients.
Other measures labelled as “lockdowns” that are milder than stay-at-home orders have contributed to all of the mentioned effects on physical and mental health too. School closures have deprived millions of children of their right to education and in poorer countries have caused hunger among children who would usually receive a meal at school. Business closures, bans on gatherings and border closures have caused an economic crisis that undoubtedly has a huge toll on people’s physical and mental health.